
By Dr Richard Maurer. Metabolic Health, Portland Maine
We can’t simply hide under the rock of being a non-smoker. I have written about medical “pre-existing conditions” and the metabolic conditions [Diabetes, hypertension, obesity] that raise the risk of severe illness from SARS-CoV-2. And there were some non-metabolic conditions I talked about, like smoking and asthma. But in the past month, these non-metabolic conditions are less of an issue. Crazy but true, Smoking history does NOT likely raise COVID-19 disease risks.

Smoking raises so many other respiratory risks that medical professional made and assumption that smoking must be a problem, but a paper in late April 2020 from UCLA states, “the current literature does not support smoking as a predisposing factor in men or any subgroup for infection with SARS-CoV-2.” Furthermore, in Paris, France, researchers published a report that opens the concluding paragraph with, “Our results suggest that active smokers may be protected against symptomatic covid-19.” I love when science challenges our faulty assumptions.
What about people with asthma? It turns out that allergic asthma is not linked to the risk of COVID-19 disease either. In late April 2020, the Journal of Allergy and Immunology published a piece where researchers posit that these patients may display reduced risk infection. [https://www.jacionline.org/article/S0091-6749(20)30551-0/pdf]
With time, as some conditions become less incriminating, the primary metabolic conditions are rising to front and center. But let’s clarify – is the risk related to diabetes type 1 or type 2? And does it matter how well or poorly it is managed?
Blood sugar management is critically important to people with type 1 and type 2 diabetes under the threat of the novel coronavirus, and tighter glucose control should be prioritized as a primary means of defense against the disease that the coronavirus causes. But this is not the medical message, is it?.
I am concerned that diabetes authorities like the American Diabetes Association misses the important message. The organization notes that poorly managed diabetes is associated with increased risks due to the accumulation of long-term damage, but doesn’t say a word about glycemic control in its “Take Precautions” page. And Coronavirusdiabetes.org, a collaboration between JDRF and Beyond Type 1, only hints at the importance of glycemic control. That website advises to “test blood sugars more often” and to “maintain blood sugar friendly eating,” without any indication that healthy blood sugars may be of newly vital importance during the pandemic.
In the meantime, the evidence continues to pile up about blood sugar control, not just a diagnosis label. A late April study published in Cell Metabolism found a truly stark difference in outcomes between patients with “well-controlled” blood glucose and “poorly controlled” blood glucose in a group of people with type 2 diabetes.
The numbers, actually, are shocking. Patients with type 2 diabetes that were unable to keep their blood sugar under 180 mg/dL (10 mmol/L) two hours after meals experienced in-lower hospital death rates (1.1% versus 11.0%) in the well-controlled group relative to the poorly controlled group.” Patients with poorly controlled blood glucose were also significantly more likely to suffer other major complications from COVID-19, including acute respiratory distress syndrome, heart and kidney injuries.
Furthermore, people without pre-existing type 2 diabetes had worse outcomes the higher their blood sugar went while in hospital. This has been attributed to a theoretical condition called “stress hyperglycemia”. But Fatty liver and insulin resistant inflammation may be the culprit in these non-diabetic metabolic cases.
I regularly hear from people who have done Blood Code screening panels and see their metabolic risks staring them in the face. I realize that when we are not sick, what’s the big deal of having a low-grade, malingering, chronic health condition. But when sick, say with SARS-CoV-2? The research of worsened COVID-19 related disease has found a link to blood test results including elevated ferritin (See Blood Code Panel #5,6,7) and elevated C-reactive protein.
The best time to act is yesterday, the second best time is now. Check out your metabolic health. We all have skin in the game to get those key metrics to look as good as possible.
Get Your HgbA1c <6.5 if you have type 2 diabetes and prevent the big swings in blood sugar – avoid getting a post meal blood sugar 160 (140-160 is the warning track)
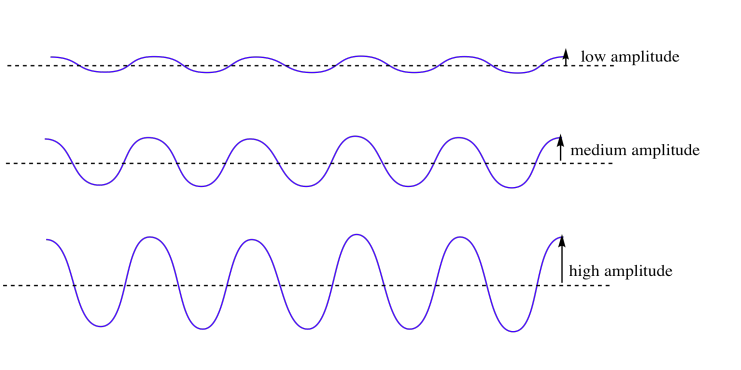
As for Type 1 diabetes, the same principle holds true, Keep fluctuations in blood sugar as narrow as possible. This requires avoiding those highly variable starchy foods like bread and pizza and sweets that spike sugar too high and require extra insulin to correct. Your blood sugar variation should be low amplitude.
For those of us without diabetes? Make sure you don’t have fatty liver, chronic inflammation, high blood sugar, insulin resistance…I could keep listing disease states but what I am looking for in myself and in my patients is metabolic health. The stakes just got higher.



Comments are closed.